Tracking mRNA from Efficacy to Effectiveness
Recent news around the promising mRNA vaccines targeting cancers results indeed caused great excitement in many circles. The number of mRNA clinical...
4 min read
![]() Karen Larimer, PhD, ACNP-BC, FAHA
:
October 20, 2022
Karen Larimer, PhD, ACNP-BC, FAHA
:
October 20, 2022

Prevention, early detection, and vigilant patient monitoring are critical elements in successfully and cooperatively managing patients with heart failure (HF).
Heart failure affects more than 6 million Americans1 and 64 million people worldwide.2 In the US, annual direct cost for HF is projected to increase from $31 billion currently to $70 billion by 2030.3 Hospitalizations represent 80% of heart failure expenditure4 – and HF hospitalization is associate with a 4-fold risk of mortality in the first 3 months after discharge.5
In a recent webinar, Josef Stehlik, MD, MPH, Professor of Medicine and Co-Chief of the Advanced Heart Failure Program at the US Department of Veterans Affairs Salt Lake City Health Care System, pointed out that, compared with the civilian population, military veterans are particularly vulnerable to heart disease. According to Dr. Stehlik, heart failure is the most common discharge diagnosis for veterans receiving care at Department of Veterans Affairs (VA) facilities.6
As America’s largest integrated healthcare system, more than 9 million veterans are enrolled in the VA healthcare system. The VA is a pioneering organization, deploying innovative digital health solutions aimed at delivering easy access and top-tier care to the men and women they serve. The VA has set goals to decrease preventable HF hospitalizations, including The Chronic Heart Failure Quality Enhancement Research Initiative (CHF QUERI) and Strategic Analytics for Improvement and Learning (SAIL).
Although people might hear “heart failure” and think of a heart attack, the clinical term actually refers to a heart that does not pump normally. A progressive disease, heart failure symptoms span a spectrum. Some patients experience no symptoms, living unaware they are at risk for an acute event sending them to the hospital. Others experience significant quality-of-life altering symptoms requiring many medications and potentially an “assist device” or heart transplant.
Medications, treatments, and devices, as well as lifestyle changes, are used to prevent disease progression and give people the best quality of life. Key to maintaining a high quality of life is good communication between the patient and their healthcare team.
Effective remote monitoring of patients with heart failure after hospital discharge could allow clinicians to safely monitor patients in the comfort of their homes and communities and identify those at the highest risk for worsening health.
Current methods, however, such as ambulatory monitoring, implanted cardioverter defibrillators and cardiac resynchronization therapy defibrillators with monitoring capabilities, or implanted monitoring devices like MEMs, either have not demonstrated clinical utility or involve expensive and invasive procedures. Therefore, an alternative like continuous remote monitoring is necessary.
Recognizing the need for noninvasive continuous remote patient monitoring for veterans with heart failure, the VA partnered with physIQ to develop a remote monitoring solution that could provide personalized alerts of potential HF exacerbation, while discharged veterans led their normal lives.
In early 2020, physIQ and the VA shared the results of a breakthrough study aimed at validating the ability to accurately predict the onset of heart failure exacerbation using wearable sensors and machine learning-based personalized physiology analytics. The solution followed veteran care from hospital to home, monitoring them 24/7 to alert clinicians at the first sign of deterioration.
With patients wearing a simple patch connected to the internet, analytics could make accurate and predictive alerts of HF exacerbation by monitoring multiple vital signs, beyond heart rate, to provide broader physiological context. The patient population in the study was representative of the typical HF patient, with a median age of 68.9 years and residing in urban, suburban, and rural settings.
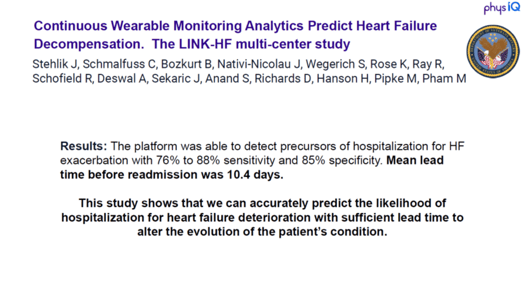
The results were impressive (see Figure 1). Published in Circulation – Heart Failure, a journal of the American Heart Association, the observational phase of the LINK-HF study demonstrated a mean lead time before readmission for a heart failure event of 10.4 days.
Figure 1. Key results from the LINK-HF pilot study.
What’s more, patients tolerated the physIQ remote monitoring very well, with only two of the 100 patients in the pilot study dropping out; demonstrating a high acceptance for a traditionally difficult-to-monitor population.
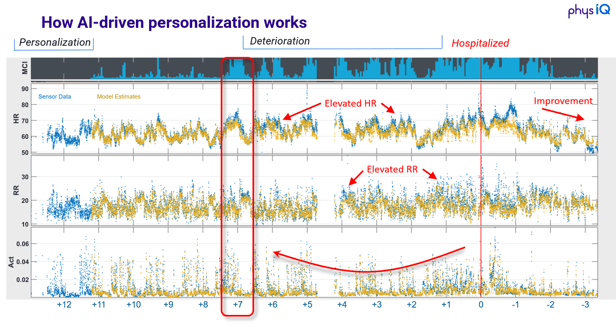
How does the technology work? In a nutshell, physIQ is able to create a personalized baseline of a patient based on their physiological data as they go about their daily activities, with a much richer data set than traditional point measurements. Once that baseline is established, deep neural nets trained on a massive data trove can detect signs of deterioration, often much earlier than the clinician or the patient themselves (see Figure 2).
Figure 2. How physIQ is able to create predictive alerts of physiological deterioration based on the patient’s own personalized baseline.
After showing promise to reduce hospitalizations of patients with heart failure, the next step was to demonstrate the value of the solution in an applied VA health program across an even broader geography and patient population that could be widely adopted as a tool to drive early interventions.
Building on this momentum, physIQ and the VA are collaborating on a follow-up study, LINK-HF2, a randomized, multicenter interventional clinical trial. This study seeks to provide further clinical evidence for the efficacy and cost-effectiveness of this approach when included in the routine care workflow of discharged heart failure patients, including fewer hospital admissions, shorter hospital stays, and better quality of life. Stay tuned for updates on the progress of this comprehensive study.
Clinical evidence is building rapidly that continuous remote patient monitoring, backed by machine learning analytics, can improve patient outcomes and quality of life while reducing healthcare costs and the burden on clinicians. At physIQ, we’re honored to be working to help our nation’s veterans and to improve global population health.
References
Recent news around the promising mRNA vaccines targeting cancers results indeed caused great excitement in many circles. The number of mRNA clinical...

The recent wave of public interest in several groundbreaking studies of mRNA vaccines in the treatment of cancer are perfect examples of how the rise...

Prevention, early detection, and vigilant patient monitoring are critical elements in successfully and cooperatively managing patients with heart...